Michael Fu, MD - HSS Orthopedic Surgeon and Shoulder Specialist
Total Shoulder Replacement - Anatomic and Reverse Shoulder Arthroplasty
Shoulder arthritis is a condition characterized by the deterioration of cartilage in the shoulder joint, leading to pain, stiffness, and reduced mobility. This condition can significantly impact daily activities and quality of life. When conservative treatments fail to provide relief, shoulder replacement surgery may be considered.
The severity of shoulder arthritis can be gauged by the intensity and impact of its symptoms, such as persistent shoulder pain that worsens with activity, stiffness and limited range of motion, swelling and tenderness around the joint, and a grinding or clicking sensation in the shoulder.
Initial treatment often involves conservative methods such as physical therapy to improve mobility and strength, non-steroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation, corticosteroid injections to decrease inflammation and provide temporary pain relief, and activity modification. If symptoms persist despite these treatments, shoulder replacement surgery may be considered.
Types of Shoulder Replacement
There are two main types of total shoulder replacement, both involving the replacement of the glenoid (socket) and ball (humeral head) of the shoulder. The two types are anatomic shoulder replacement (or arthroplasty), and reverse shoulder replacement. Historically, the majority of shoulder replacements performed were of the anatomic variety. Over recent years, however, reverse shoulder replacement has become much more common than anatomic shoulder replacement, accounting for approximately 70 to 80% of shoulder replacements in the United States.
Anatomic Total Shoulder Replacement
Anatomic shoulder replacement, a traditional approach, involves replacing the damaged parts of the shoulder joint with artificial components that mimic the natural anatomy of the shoulder. In this surgery, the damaged humeral head (the ball of the shoulder joint) is replaced with a metal ball, and the glenoid cavity (the socket) is lined with a durable plastic component.
Anatomic total shoulder replacement
This procedure is best suited for patients with intact rotator cuff tendons, joint damage primarily confined to the ball and socket of the shoulder joint, and patients with minimal bone deformity, particularly of the shoulder socket.
The primary goal of anatomic shoulder replacement is to restore the natural structure of the shoulder, thereby improving function, reducing pain, and maintaining the range of motion. Again, it is most effective in patients whose rotator cuff muscles and tendons are healthy and functional. An important consideration for anatomic shoulder replacement is that if the rotator cuff tendons were to tear or fail in the future, the shoulder replacement would no longer function well, and patients may require additional surgery.
Reverse Total Shoulder Replacement
Reverse shoulder replacement is a more recent innovation designed to address conditions that traditional anatomic replacement cannot. In this procedure, the natural positions of the ball and socket are reversed: the metal ball is attached to the shoulder's socket, and the plastic socket is affixed to the upper arm bone (humerus).
Reverse total shoulder replacement
This design is particularly beneficial for patients with rotator cuff tear arthropathy, complex fractures of the shoulder joint, previous unsuccessful shoulder surgeries, severe arthritis with rotator cuff tears, and significant bone deformity of the shoulder socket.
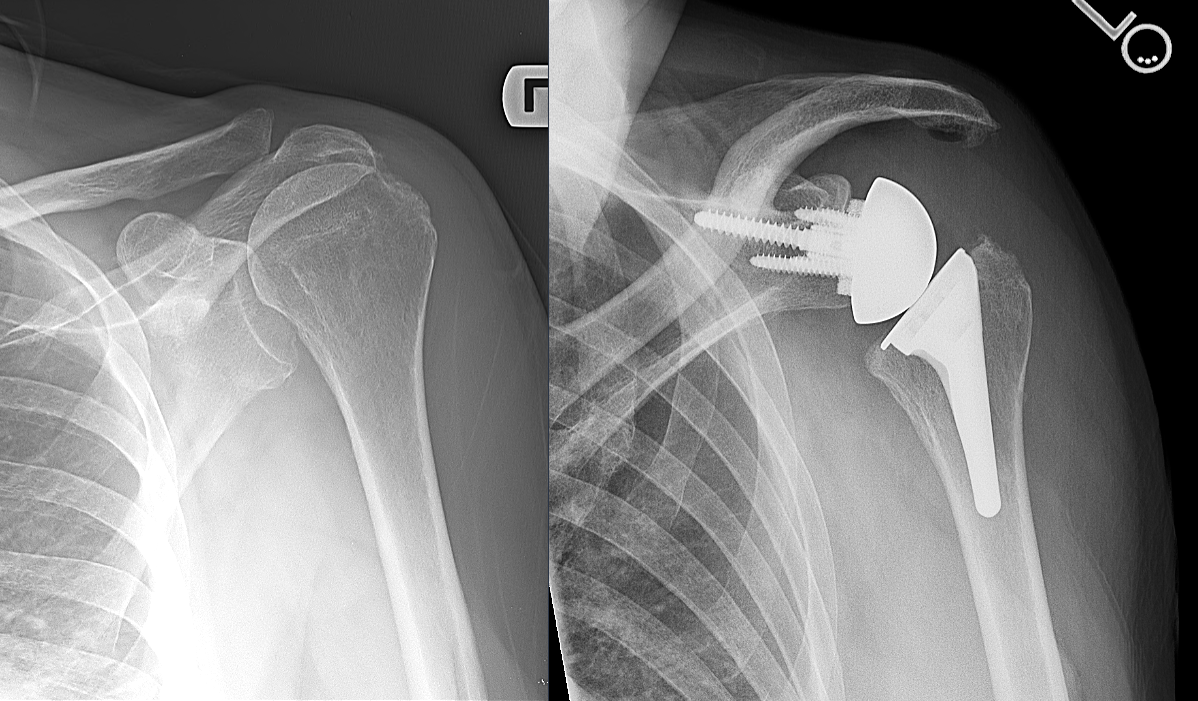
Shoulder rotator cuff tear arthropathy before and after reverse total shoulder replacement
The reverse design allows the deltoid muscle, rather than the compromised rotator cuff, to power and move the arm. This procedure is especially advantageous for those who lack the functional rotator cuff necessary for an anatomic replacement, offering them a significant reduction in pain and improved arm function. The reverse shoulder design is also more congruent and stable than the anatomic design.
Choosing Between Anatomic and Reverse Shoulder Replacement
The decision between anatomic and reverse shoulder replacement hinges on several factors, including the patient's specific shoulder condition, the integrity of the rotator cuff, and the desired outcome of the surgery. Anatomic replacements are favored when aiming to maintain the shoulder's natural mechanics in the presence of a healthy rotator cuff. Conversely, reverse shoulder replacements are selected to leverage the deltoid muscle for shoulder movement, especially in cases where the rotator cuff is severely damaged or non-functional.
Even in patients with relatively straightforward arthritis and an intact rotator cuff, emerging research is underway to compare patient outcomes between anatomic and reverse shoulder replacement. Even if the rotator cuff is intact, the natural history of the rotator cuff is that it will continue to degenerate and tear as patients age. Therefore, some patients may be recommended for a reverse shoulder in this scenario to avoid the need for revision surgery if and when their rotator cuff deteriorates in the future. Therefore, the vast majority of shoulder replacements performed in the United States currently are reverse total shoulder replacements.
Conclusion
Both anatomic and reverse shoulder replacements offer valuable solutions for restoring shoulder function and alleviating pain with end-stage shoulder pathology. The choice between these surgeries depends on individual patient assessments, with the primary considerations being the state of the rotator cuff and the specific nature of the shoulder's dysfunction. Please contact our office for a consultation to determine the most appropriate treatment plan for individual cases.
About the Author
Dr. Michael Fu is an orthopedic surgeon and shoulder specialist at the Hospital for Special Surgery (HSS) in New York City (NYC) and New Jersey (NJ), the best hospital for orthopedics as ranked by U.S. News & World Report. Dr. Fu is an expert at shoulder rotator cuff repair surgery, shoulder instability surgery, and shoulder replacement. Dr. Fu was educated at Columbia University and Yale School of Medicine, followed by orthopedic surgery residency at HSS and sports medicine & shoulder surgery fellowship at Rush University Medical Center in Chicago. He has been a team physician for the Chicago Bulls, Chicago White Sox, DePaul University, and NYC’s PSAL.
Disclaimer: All materials presented on this website are the opinions of Dr. Michael Fu and any guest writers, and should not be construed as medical advice. Each patient’s specific condition is different, and a comprehensive medical assessment requires a full medical history, physical exam, and review of diagnostic imaging. If you would like to seek the opinion of Dr. Michael Fu for your specific case, we recommend contacting our office to make an appointment.