Acromioclavicular (AC) Joint Arthritis
Michael Fu, MD
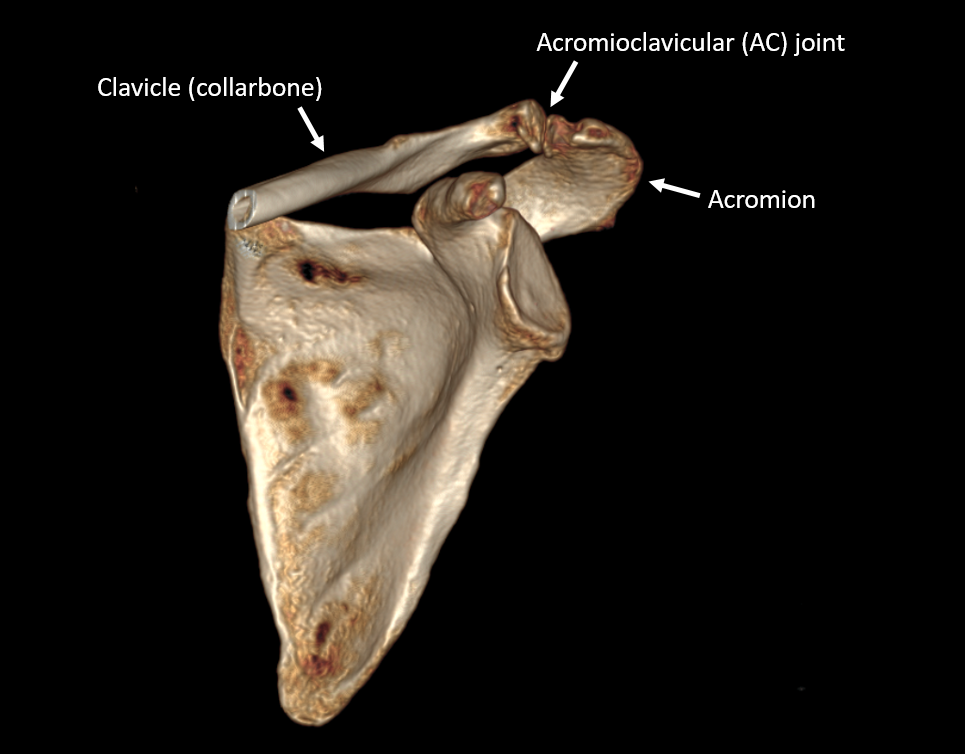
The acromioclavicular joint, or AC joint, is where the end of the clavicle (collarbone) meets the top of the scapula (shoulder blade), at a curved piece of bone called the acromion.
The AC joint is surrounded by a thick joint capsule, and is also stabilized by the coracoclavicular (CC) ligaments as well. When these soft tissue structures are injured, typically through sports injuries or trauma, then an AC joint injury (also known as a separated shoulder) may occur. AC joint injuries are beyond the scope of this article, but they may predispose someone to developing AC joint arthritis down the line. In addition to post-traumatic causes, AC joint arthritis may also develop from simply years of normal shoulder-related wear and tear. Activities such as reaching across your body and laying on your shoulder can lead to significant forces across the AC joint.
Presenting symptoms
Patients with AC joint arthritis typically report pain directly over the AC joint, at the top and the front of the shoulder. This area will be tender to palpation as well. These symptoms commonly occur concurrently with other shoulder conditions, such as rotator cuff tears, subacromial bursitis, and biceps tendinitis. In this setting, it may be helpful to be evaluated by a shoulder specialist who is trained at differentiating the various sources of pain around the shoulder to arrive at the most appropriate diagnosis and treatment. Patients often report that their symptoms are made worse by reaching across their body, and laying on their side with the affected shoulder down. This can lead to significant night pain and poor sleep in patients who like to sleep on their side.
Non-operative treatment
We recommend beginning with non-surgical treatment for symptomatic AC joint arthritis. Treatment may include activity modification, physical therapy, and oral anti-inflammatory medications (NSAIDs, such as ibuprofen, naproxen, meloxicam, etc.). If symptoms continue to persist, then an ultrasound-guided injection of cortisone into the AC joint may be considered as well. This type of injection can be used for both diagnostic and therapeutic purposes, as a way of determining how much of your shoulder pain is coming from the AC joint.
Operative treatment - AC Joint Resection
If AC joint arthritis continues to be symptomatic despite trying the non-operative treatments above, then surgery may be considered. Since AC joint arthritis commonly occurs concurrently with other shoulder conditions, we generally try to address all symptomatic shoulder issues in a single surgery.
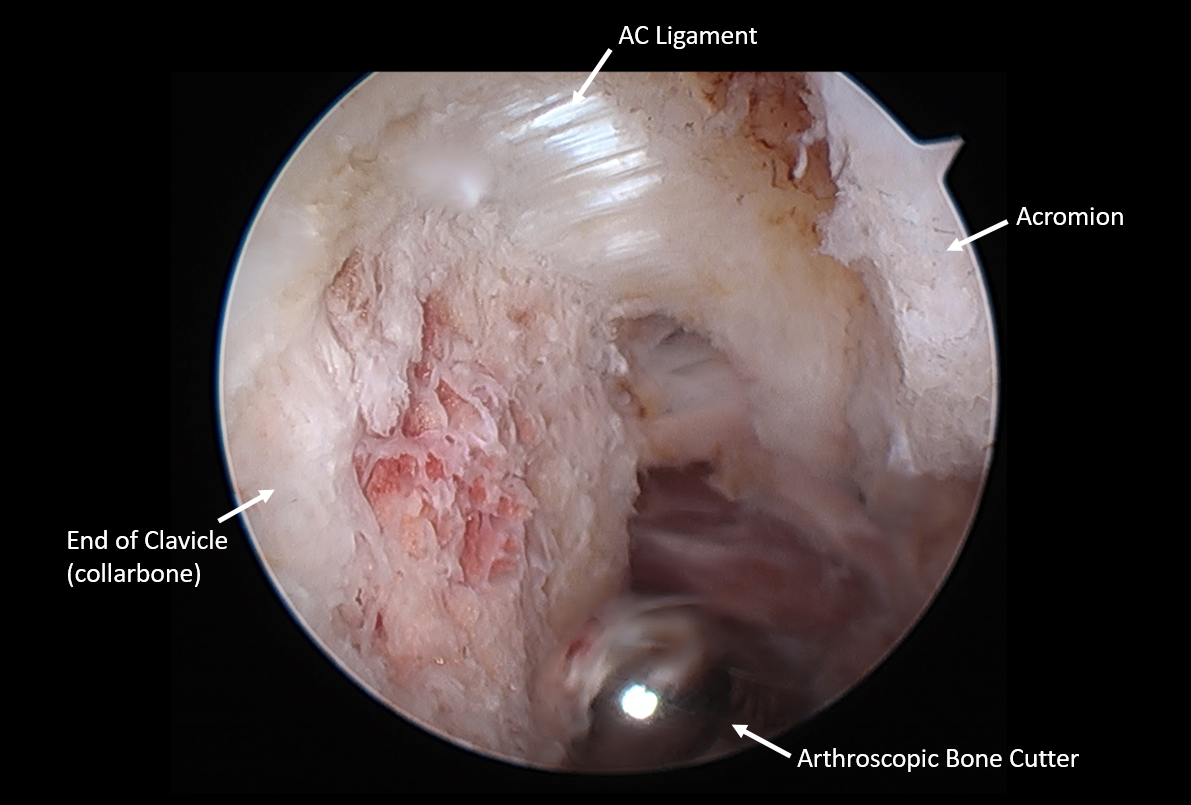
Surgical treatment for AC joint arthritis can be performed through a minimally-invasive arthroscopic approach. This involves exposing the undersurface of the AC joint, and removing all inflamed and diseased tissue from the joint. The bony articulation of the AC joint is then removed, mostly from the end of the clavicle (collarbone), so that the clavicle and acromion are no longer touching. Care must be taken to preserve the soft tissue stabilizers of the AC joint so that instability does not become an issue after surgery.
Arthroscopic surgery for symptomatic AC joint arthritis. The end of the clavicle (collarbone) is resected so that it is no longer touching the acromion on the other side of the arthritic AC joint. Note that the AC ligament must be preserved to avoid post-operative instability.
As always, each patient’s case is unique, and we hope this information is helpful for gaining an understanding of AC joint arthritis and potential treatment options. We would be happy to consult with you virtually or in-person, to review your situation in detail and answer all of your questions.
About the Author
Dr. Michael Fu is an orthopedic surgeon and shoulder specialist at the Hospital for Special Surgery (HSS) in New York City (NYC) and New Jersey (NJ), the best hospital for orthopedics as ranked by U.S. News & World Report. Dr. Fu is an expert at shoulder rotator cuff repair surgery, shoulder instability surgery, and shoulder replacement. Dr. Fu was educated at Columbia University and Yale School of Medicine, followed by orthopedic surgery residency at HSS and sports medicine & shoulder surgery fellowship at Rush University Medical Center in Chicago. He has been a team physician for the Chicago Bulls, Chicago White Sox, DePaul University, and NYC’s PSAL.
Disclaimer: All materials presented on this website are the opinions of Dr. Michael Fu and any guest writers, and should not be construed as medical advice. Each patient’s specific condition is different, and a comprehensive medical assessment requires a full medical history, physical exam, and review of diagnostic imaging. If you would like to seek the opinion of Dr. Michael Fu for your specific case, we recommend contacting our office to make an appointment.